Chemotherapy
Meeting the Oncologist, 29 March 2019
I had my first meeting with the oncologist and I now have a treatment plan for my chemo. Apparently there are two different treatments for my cancer. The better version is more aggressive and is only tolerated by one in twenty patients. So, as one of the younger victims, I've been nominated for best of class treatment and will undergo MVAC chemotherapy. The letters in this acronym stand for four different chemical with impossible names. I've decided it stands for "My Very Aggressive Chemo".
MVAC is administered in two steps. I'll get M on Thursday during a one hour session, and VAC on Friday during a five hour session (yes, five hours of chemical warfare). This process is repeated four times every two weeks. The only exception will be the last round. It will be delayed by another week so I can attend my son's college graduation ceremony.
So the good news is that everything will go faster than expected and the outcome will be better. The disadvantage is that it will be more miserable. It also means that my bladder removal and reconstruction surgery will also be sooner than expected.
The Week before Chemo, 3 April 2019
Apparently Mr. Murphy is never far away. About 10 days before my first round of chemo, I started to have pain in my urinary tract. Initially this was dull but it became so bad that I cold no longer sit or lay down without major discomfort. To make matters worse, my wife and I had planned a trip to see our kids (who are in college) before chemo starts, and although it was great to see them, the pain was dominating the whole trip.

On the way back home, I noticed that my urine was also very cloudy which made me believe I had an infection. Quickly playing Dr Google confirmed that all my symptoms lined up with a UTI. Given that I still had antibiotics left from that long "none prostatitis treatment", I decided to self medicate (kids listen to me, never do this at home). With long chemo sessions around the corner, it was important that I could sit without discomfort so I decided to see the urologist or a RN.
Sure enough they found a "mixed fauna" in my urine but not enough to conclude it was a UTI. Luckily, the RN did prescribe more antibiotics and the pain stopped just in time for chemo round one. I clearly dodged that bullet even though they did not think it was a UTI. Obviously I did not tell them about the self medication.
Chemo Round One, 8 April 2019
Last week, I had to complete three things before I started my chemo. Firstly I had to get a PICC line installed. This is a permanent port they use to draw blood and inject the chemicals. The line starts in your arm and ends just before your heart so the chemicals are immediately dispersed through your entire body. The other advantage is that they don't have to poke you every time. It will stay there for 8 weeks.
The second thing was a 45 minute heart echo. My CT scan and EKG had shown that my heart was good, but the oncologist wanted to make sure it could handle the nasty stuff. I passed that test with flying colors and the nurse even joked that I could make money on the side modeling my heart.
The last bit was the chemo training. This was very useful as a nurse explained the process, the chemicals, and the do's and don'ts. So to my surprise, I'm not just doing the 1 in 20 MVAC, I'm doing the accelerated or "dose dense" version. Normal MVAC is every 4 weeks, the accelerated version is every 2 weeks (lucky me). The sales pitch is that your body has less side affects if you do it faster (don't ask me about that logic).
So right after the chemo training, I entered the chemical warfare room and got my M chemical. Not a big event as it was over in 30 minutes with no side effects. On Friday however, I did my VAC chemicals which was advertised as 5 hours. Just like any good airline, we had some delays and the entire journey took 6 hours and 45 minutes.
The amount of stuff they put in me was ridiculous (it must have been over 3 liters). First saline to hydrate me, then anti-nausea medication followed by a bag full of steroids. Finally it was time for the V chemical. At this point, three nurses showed up with a box full of bags (everything I needed for the rest of the treatment) and they spent 5 minutes checking serial numbers, quantities, expiration dates and matches with my wristband. Given that this stuff is nasty and dangerous, I had to appreciate their attention to detail but at one point, I could not help myself and feel like a prisoner on death-row.
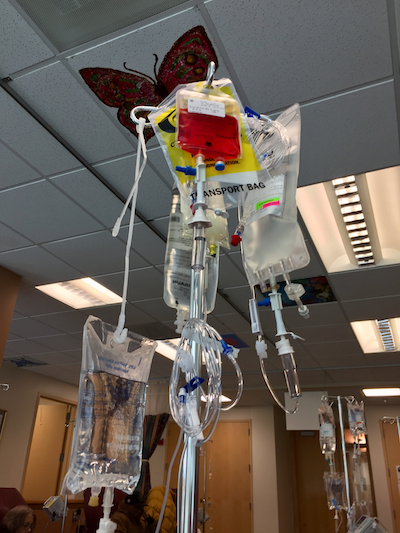
The A and C chemicals are really bad apparently as my kidneys had to be flushed with 1 liter of saline after the A and half a liter of the C to avoid damage. So after almost 7 hours I left the place and although I was tired of sitting, I did not feel any different.
All of this changed on Saturday when my energy level went down very quickly. By the time Sunday came around, I was hitting a wall and was sleeping most of the time. Monday morning I started to feel better although the progress was very slow.
The best way to describe the treatment so far is to be hit by the worst flu ever but without the fever. Every muscle and joint aches, you have a slight headache, no energy or appetite and you sleep a lot. Nausea was minimal but the additional pills they gave me, controlled it nicely. The biggest issue I have right now is that I can't concentrate. A five minute conversation knocks me out.
So overall as the optimist, I can't complain too much as many people have far worse symptoms. I know I still have three sessions to go and think it will still get worse. Nevertheless, I still feel good about the outcome. I did not pick this fight but I will win this war.
Recovering from Chemo Round One, 17 April 2019
Recovery from the first round of chemo has been a rollercoaster. Four days after the chemo session I started to feel better, but good and bad days would alternate for another 4 days. It wasn't until one week after the chemo that I really improved and was eating well again. Actually, I was eating so well that I even gained weight.
We were told that I would most likely not lose all my hair but that it would thin out. This did exactly happen during the first round of chemo. When I washed my hair, little bits came out but not much. The other noticeable thing is that my hair is getting thinner and softer, and my facial hair has decided to slowdown growth. Less shaving for me for a while.
Chemo Round Two, 23 April 2019
One day before the second round, I had to do blood work to see how my body recovered from the first round. I passed that test with flying colors, so I'm ready for round two.
The other good news was that I could move my chemo treatments to 8 o'clock in the morning, right as the office opened. The good part about this is that the doctors don't start working until 9 o'clock so the waiting rooms are empty. I think I was patient number three so from the moment I got into the building, I was hooked up to my lovely concoctions within 10 minutes. The entire process took less than 5 hours which was a vast improvement over the 6 hours and 45 minutes of the first round. I've scheduled rounds three and four at 8 o'clock as well.

Round two was different from round one. This time there was no honeymoon period as my body immediately recognized what was happening and even on the Friday a few hours after the treatment, I already started to go down.
Tiredness, muscle and joint aches, lack of concentration and that general flu sensation were the same. What was different was the nausea and I was not able to control it with medication on Sunday or Monday. Luckily, Tuesday morning things turned around and I started to feel a little better. In under 3 days I lost 5 pounds and a lot of hair.
Hopefully I can strengthen over the next 10 days so I'll be ready for round 3.
Recovering from Chemo Round Two, 26 April 2019
Round two has been different than round one. This time there was no rollercoaster but the intensity was greater in terms of tiredness and nausea. One week after the chemo, I can clearly feel my strength coming back and I have yet again some color in my face. I assume my white blood cell, red blood cells and platelets are making a strong comeback.
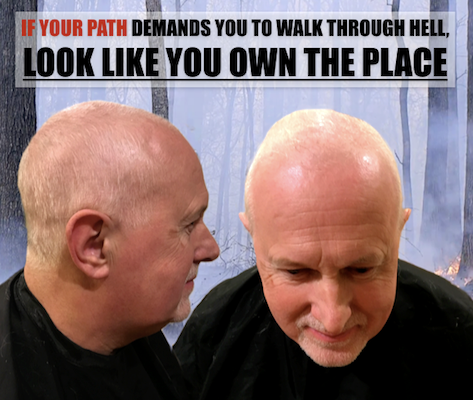
The biggest difference however has been my hair as I started to lose it rapidly leading me to take drastic hairstyle measures. Funny enough, it only affects hair on top of my head and the rest of my body is (still) normal.
PICC Line Drama, 27 April 2019
As I mentioned earlier, I had a PICC line installed in my upper left arm. This line is nothing more than a small tube that enters my upper arm and runs to my heart so that the dangerous chemicals can be distributed quickly through my entire body instead of lingering near an entry point where they could potentially damage tissue. The only thing that sticks out of my body is a small tube with a port on it that they connect to an infusion line when required.
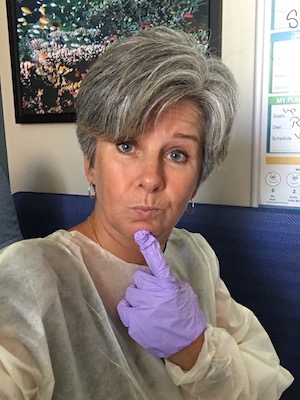
Every week on Wednesday, the entry area has to be disinfected and they put a very sticky antibacterial gel and a see-through cover on it so the entry wound can be monitored easily. White mash netting that looks like a bandage is put over the whole thing to hold the dangling port in place. As I don't feel or notice it much, I got into the bad habit of not checking the entry wound every day.
Today as I took a late shower, I noticed a lot of blood around the wound covering the entire area of the clear bandage. This spooked me a little and had to seek help immediately. With my luck, it was now Saturday evening and the only option was an Emergency Room (ER). Luckily it was early in the evening so the ER was still quiet. The crazies, the intoxicated and the gunshot victims would likely arrive much later.
After being checked by multiple doctors and nurses, they concluded that the clip on my arm that holds the line in place was not mounted properly during Wednesday's cleaning and caused the line to move a little and start the bleeding. Remedy was simple: take all the stuff off, clean it well and reapply new disinfectant gel and cover it back up.
Well, that was easier said than done as the ER did not have the kits to treat PICC lines available and none of the nurses had actually done it. Problem one was easy to solve. The infusion center that cleans my PICC line is literally next door to the ER and it's operated by the same organization. Problem was that it's locked. Luckily an American ER has security guards on duty to deal with out of control patients and I was able to convince the nurse to convince the guard to break into the infusion center and get the right supplies.
The second problem was more interesting. The nurse who did the cleaning had only seen a PICC line in training many years ago and wasn't too comfortable. As I witnessed 5 cleaning sessions already, I was able to coach her through the process and get all the right bits in the right place while keeping everything sterile. Lesson learned: always look at medical procedures performed on you. You never know who you might have to coach through the process.
Hair Style Fun, 28 April 2019
After I posted my new "badass" hairstyle on the blog, I got a lot of very nice reactions that, for a bit, drew attention away from my war on cancer.
The first good reaction came from a dear friend in California. She noted that I totally ROCKED the new style and that I looked like a badass MARINE or NAVY SEAL. Luckily her husband stepped in quickly and put the word (RETIRED) in that sentence followed by another friend pointing out that I might look like a Navy Seal but not the one that's on trial for war crimes. Thank goodness for that clarification.
My family in the Netherlands had a different view as they compared me to rock stars like Peter Gabriel and Billy Joel. If you read my main web page, you quickly realize how fitting that was.
My own children, who used to binge watch Breaking Bad on Netflix, saw a resemblance with the lead character Heisenberg (but without the meth lab off course). As a result, I'm no longer a "badass" but rather a "Breaking Bad ass". This inspired my wife to take the appropriate pictures.
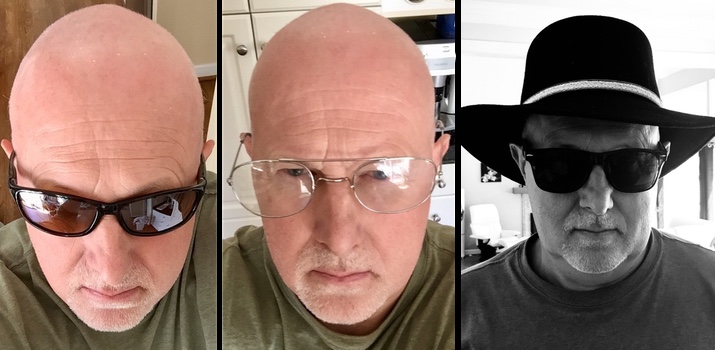
So in a few simple days I went from just another guy with cancer, to a badass (retired) Navy Seal (that did not commit war crimes), to an aging rocker, to a Breaking Bad Ass. Not a bad three day transformation.
Chemo Round Three, 1-10 May 2019
From the beginning, I was told that successive treatments would be worse in terms of side effects. I my case, this is definitely true as I hit deeper lows that also lasted longer. In order for this blog to be useful to future patients, I'll give a day by day summary of my round 3 journey so other people can benefit form it later.
- 1 May - This is the day before the two day treatment and my body already knew what was coming. Most of this is a mental game with physical side effects. When I did round 1, I didn't know what to expect. Round 2 was worse (certainly in terms of nausea) so now my mind is wondering how bad it will get in round 3. Stupidly enough, I already started to feel queazy before a drop of chemicals was administered as the mind was dominating the body.
- 2 May - Day 1 of treatment started with a blood test, followed by a consult with a physician's assistant, followed by treatment with the M chemical. The results of the blood test were good with the exception of white blood cells. Instead of them being a little low, they were actually a little high which could indicate an infection. As I did not have a fever, they didn't seem to be too worried but in an abundance of caution, they put me on five days of antibiotics anyway. The pre-drama queasiness continued, reenforcing the notion that it truly is mind over matter.
- 3 May - Day 2 of treatment started really bad as I did not sleep very well. I think there was an element of anxiety and nervousness but I basically started the day with nausea before the drugs were even administered. The one good thing about been tired is that I slept through most of the 6 hours of treatment with the VAC chemicals but when I came home I was exhausted and the queasiness became worse. I could feel a very fast downward trend coming up. May 3rd is also our 31st wedding anniversary. My wife and I agreed to celebrate double next year.
- 4 May - Going down hard! As described earlier, it's mainly a bunch of flu symptoms like muscle aches, painful joints and general tiredness. The difference with the flu is that the symptoms seem to be more severe. Sleep is the only remedy.
- 5 May - Here comes the nausea! This was a really bad day as I couldn't eat or drink anything and I could feel a strong mental decline. People around me want to help me so badly but even their attempts were hard to handle. I just wanted to be left alone even though it is very hard to send away loved ones that just wanted to help.
- 6 May - This was by far the worst day of round 3. The discomfort in terms of tiredness, muscle and joint aches, nausea and lack of energy continued. This was probably the first day in this journey where I lost my positive attitude. It was so bad that my stupid brain couldn't even see how this could ever get better. On top of that, I still couldn't eat or drink, making my situation probably even worse. This was one of those days where you could hear people say with sufficient drama: "if this continues, I would rather die".
- 7 May - Physically, I think this was the day things started to improve slowly. Mentally though, my brain didn't spot this yet as I was too busy feeling sorry for myself. Luckily, I did sleep a lot so the day went by quickly.
- 8 May - More improvements were now noticeable and I started to come out of my mini depression. I did however have to distract myself as any reminders of cancer, chemo or the treatment made me feel physically ill.
- 9 May - Hope and a positive attitude came back as the improvement are now coming a little faster. I slept a lot less and had my first decent food in a few days.
- 10 May - This day I was supposed to attend the farewell lunch of one of my dearest colleagues at an Indian restaurant. Normally, I would be the first to show up for a spicy curry but the notion of Indian food smells was so off-putting that I had to cancel my participation. Overall physical and mental improvements are there but not as fast as I would like them.
- 11 May - This was the first somewhat normal day in round 3. I had regular (small) meals, slept for only 30 minutes during the day and the tiredness was bearable.
- 12 May - After neglecting this blog for almost 2 weeks, I finally had enough energy and sufficient attention span to write a few entries. Even thinking about this blog triggered queasiness. I now have one week to get strong enough for my son's graduation and 2 weeks before the final (and probably most awful) round of chemo.
PICC Drama, the Sequel, 9 May 2019
I'm not having much luck with my PICC line. Yesterday was my weekly PICC line cleaning and while taking a shower just before I went to the Infusion Center, I noticed that my left arm was swollen and discolored. The entire arm was more red with a purplish hint. Clearly this was not a good sign and on top of it, the area around the PICC line entry wound looked more red than before.
The nurse at the Infusion Center was very good and took action immediately. She got the opinion of a few other nurses and then decide to call my oncologist directly. Collectively they decided that there was a risk of an infection or even blood clots. My oncologist told the nurse that he would order an ultrasound of my arm and some other tests to see what the problem was. I should be contacted within 24 hours. The nurse did clean the area just in case and put on a clean bandage.
As I mentioned before, I've been very happy so far with the medical treatment but the administrative side remains an abomination. As expected (and even predicted by my good nurse), I never got a call so I had to become proactive again. As usual, it was hard to get passed the automated telephone system and the unpleasant pitbull operators but I managed to get in touch with a scheduling secretary as well as a triage nurse. True to form, the secretary was useless and even rude while the nurse was helpful and saw the potential dangers. I had an appointment within 2 hours.
Medical staff quickly took my vitals and ruled out an infection due to the normal temperature and other vital signs. The ultrasound of my left arm did however show that I had two blood clots. One in my upper arm and one in my armpit. Unfortunately, Thursday is the day off for my oncologist but the nurses tracked him down somewhere on a golf course and got his guidance. These nurses are saints and if the administrative staff was half as human as them, the world would be a better place.
The doctor's recommendation was not to panic, put me on blood thinners for 3 months and monitor closely. "3 months", I asked? I never got a good answer but I suspect the pharmaceutical industry is behind it as this new drug that I was given is expensive. They gave me 30 days free (a $950.00 value) so they clearly have to recoup their "generosity" in the following months. Who knows what the second and third month will cost? Good news for me is that my bladder removal and reconstruction is within this time window and they clearly don't want you to be on blood thinners during 9 hours of internal surgery. Hopefully, these blood clots don't mess up my schedule as it's starting to look like I spent more time on side effects of side effects rather than dealing with the real problem. It would be highly ironic if you die from a side-effect's side effect when trying to save your life from an aggressive cancer.
The one remaining issue was the red area around the PICC line. Given that there is a three week window between chemo rounds 3 and 4 (due to my son's university graduation), I was in no mood for more risks. Imagine another complication on graduation day? No, thank you. I therefore convinced the nurses to remove the PICC line and accept having to get a new one installed just before chemo round 4. The nurses thought this was a great plan but needed approval from the oncologist. His golf game got interrupted again and he agreed.
Update (3 days later): The PICC line removal was simple and painless. I did have some bruising for a few days but that was to be expected as they use serious pressure to stop the bleeding. The entry wound is healing quickly and the redness is almost gone.
More Side Effects, 13 May 2019
Well, I concluded too quickly that I was done with side effects. The medication prescribed to treat my blood clots caused my bladder to bleed again. Because of all my kidney stones, I had learned that it doesn't take much blood to make it visible in your urine. My urine however wasn't just tinted red, it was red and looked like pure blood (a slight dramatization).
So here comes "Deja Vu all over again". I first called the urologist and was once again greeted by an automated telephone system and unpleasant pitbull operators. They told me it was not possible to just walk in and I would get a callback from a nurse. My second course of action was to call the oncologist and with a little extra drama in my voice, I was able to talk to the triage nurse and was asked to come in immediately.
As always, the oncology medical staff was efficient and very helpful. Not only did they think that the bleeding was exacerbated by the blood thinners, they actually suspected a Urinary Tract Infection (UTI) as my white blood cell count was very high. I was again put on antibiotics and they reduced the blood thinner dose. Within 4 days the bleeding stopped and the discomfort went away. Later the oncology staff confirmed that I had a UTI based on a urine culture test.
Eventually, 3 days after my first call, I got a callback from a urology nurse. I was not amused and let her have it over the phone. How come I had to go to an oncologist with a urology problem? Why did I almost go to an emergency room to have a doctor there call the urologist and get his attention? The nurse was shocked by the treatment I received from the admin staff and told me that in case of emergency (and bleeding is clearly one of them), I should always come to the office and would be helped immediately. Apparently the admin staff has quite a reputation and the nurse promised me she would raise this issue (again) with the office manager. I thanked her for her effort but told her that I would not be holding my breath.
My Son's College Graduation, 18 May 2019
When I started chemotherapy, I knew that my son's college graduation would be somewhere in the middle of it. Luckily my oncologist understood the importance of that day and scheduled the chemo in such a way that on graduation day, I would be the best I could be. This is the reason why there was a three week break between chemo rounds 3 and 4 as compared to the usual 2 weeks called for by the dose dense MVAC protocol.
Graduation day was two weeks after round three and I felt pretty good. Our San Diego friends (who are our son's godparents) also came and we had a great weekend together. I was able to participate in all activities and enjoyed all of them. Having your first child graduate from college is a big deal and we were very proud of our son who graduated with a double Bachelor's Degree in Communications and Film.
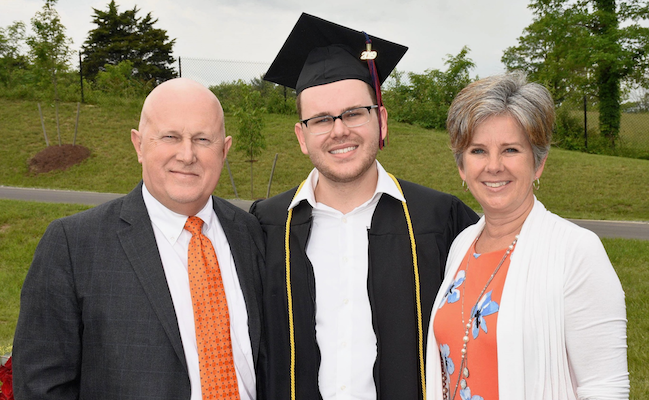
Because of the severity of round three, I must admit that prior to the graduation, my mental state had taken a beating. The hopeless optimism that I had at the beginning of chemo wasn't as strong anymore which really bothered me during this special weekend. Having had kids in my late 30s, I recognized that many key family milestones were still to come like our daughter's graduation, marriages and possibly grandchildren. I assume every cancer patient has these moments where thoughts about future ambitions and mortality cross paths. What if I'm not around for those special moments? How would the family handle my absence? What will their lives look like?
I quickly realized that this line of reasoning causes a downward spiral into anxiety and depression. Luckily I was reminded of a former boss and his words of wisdom. General James Mattis is probably one of the most remarkable people I've ever met. He is a tough as nails Marine with an exceptional intellect and memory (don't play trivial pursuit with him) and an unbelievable sense of compassion. I decided to borrow one of his famous quotes and give it a twist in an open letter to "cancer". It definitely stopped my mental death spiral in its tracks and I'm now more ready for the fourth and final round of chemo.
Dear Cancer,
I've come in peace without an army as I simply want you to leave my
body. But I'm pleading with you, with tears in my eye: If you keep
fucking with me, I'll have to kill you all.
Johan
Urology Visit, 22 May 2019
After three rounds of chemo, my urologist wanted to look at my bladder to see how the treatment was progressing by performing a cystoscopy. Well, this did not work as planned. I already mentioned earlier that I have scar tissue in my urethra (called a urethral stricture) from kidney stone removal surgery in the early 90s. As it turns out, I now have another stricture caused by the second biopsy and bladder resection surgery. I don't notice this when going to the bathroom but this one is so bad that the urologist could not get the scope into my bladder. Given that it is the same guy that caused the problem, he wisely decided not to force it and avoid unnecessary torture. He will now use the upcoming CT scan with contrast fluid to determine the effectiveness of the chemo treatment.
I was obviously OK with not doing the cystoscopy but the new stricture might have an effect on my bladder reconstruction surgery. Depending on how narrow my urethra has become, a neobladder might not be the best option as I might not be able to push the urine out with my belly muscles. This would be a setback but a final decision is not required until late June. More stuff to worry about next month.
PICC Line 2.0, 23 May 2019
To go through chemo round four, a new PICC line had to be installed as two of the four chemicals are too toxic to put straight into a vain. Given how easy it was to install the first PICC line, I thought it would be a piece of cake to install version 2.0. Well, I was greatly mistaken.
A PICC line is inserted into your upper arm and runs to near your heart so the chemicals can be dispersed to your entire body quickly. Clearly this is a risky process as you might infect your bloodstream or damage major arteries. As a result, the procedure is performed in an Operating Room (OR) under sterile conditions. The anesthetic (novocaine, the same stuff used by a dentist) is applied locally on your arm and you can follow the whole process as you are awake. The OR is equipped with two tools. Firstly, an ultrasound machine to see where the arteries run in your upper arm and to ensure the needle hits them. Secondly, a live low-dose x-ray machine to see how far the guide wire is from your heart, allowing staff to cut the PICC line to perfect length.
So for my first PICC line, I went to the hospital where I was greeted by a very large male nurse who took me to the OR and got me ready. He was very kind and soft-spoken but did not waste any words. Within 5 minutes, two additional male nurses arrived. This was "straight-from-a-horror-movie" scary as the two individuals were also very large, unshaven and they looked like they just escaped from Alcatraz. These two did not waste any words either and went straight to work. The team was all business and the whole process took than less than 10 minutes. Before I knew it, I was on my way home. No pain, no discomfort, just a tube sticking out of my arm.
The second PICC line was installed at a different hospital. This time there were no scary men in sight and the prep area as well as the OR were overstaffed with very friendly female nurses. They took almost an hour to get me ready and finally wheeled me into the OR. At that point I should have known this was not going to be the same as the first experience as the nurses (all five of them) where constantly talking about their private lives. As a patient, you can see the ultrasound and x-ray machines (if you care to look at it) and I quickly noticed that the first attempt with that large needle did not hit the vain. Neither did the second but these failures were covered up by all the private smalltalk. During attempts three and four, they decided to poke around a little which really hurt. Novocaine was added about 5 times. After four botched attempts, I pointed out that the team that successfully did the first PICC line used a different vain (just look at the scar on my other arm). Begrudgingly they accepted my point and successfully installed the new PICC line on the fifth attempt.
Below is a picture showing the immediate aftermath with a PICC line on top of my arm and the "near misses" on the side of my arm. This entire area turned purple and black for almost two weeks. Next time, I'll try to find the escapees from Alcatraz again.

Chemo Round Four, 23 - 24 May 2019
Hallelujah, we're there! Here comes the last round of chemotherapy. As expected, the cumulative effect of multiple rounds of poison was noticeable especially in the tiredness department. The progression of round four was about the same as round three (which I chronicled in detail below) but I got a lot more tired than before.
The big difference with the other rounds was nausea. In rounds two and three I suffered from "traditional nausea" with classic symptoms such as an upset stomach, queasiness, faintness, dry mouth and diarrhea. All of this was controllable with medication and looking back at it, it was manageable.
The new thing in round four was what I would call "mental nausea". For no good reason, thinking about chemotherapy, smelling something that reminded me of chemotherapy or seeing an object that I associated with chemotherapy caused an immediate and violent reaction. Within minutes, I would throw up followed by at least another ten or twenty gag reflexes to the point that my entire body would hurt.
The first time this happened was two days before round four. I was about to go to bed and was cleaning my contact lenses. All of a sudden, I had to think about the upcoming round four and within minutes, I got very sick and started to vomit. The second time it happened was in the oncologists office where it's very hard not to think about chemotherapy. In total it happened about five times and all episodes were equally dramatic. It wasn't until two weeks after round four that it stopped.
When I got physically stronger, it allowed me to become mentally stronger and have better control over these negative effects. The other thing that might have helped is a change in mindset. When I started chemo, I took the advice to listen to my body which served me well. When the mental nausea got really bad, I decided to reverse this logic. I was done with chemo and to heal faster, I thought it to be better for my body to listen to me. It actually worked as I recovered faster and the mental nausea went away.
I guess the entire episode proves that the brain is a powerful organ. It was capable of making me physically ill based on a simple thought but it was also capable of accelerating my healing based on positive willpower. I guess the big lesson learned here is that I should have worked more on mental health when going through chemotherapy. I need to keep this in mind for the upcoming surgery.
Happy Birthday, 3 June 2019
Ten days after chemo round four was my 59th birthday. As this was not the best time to celebrate, I decided to officially move my birthday to June 16th (Father's Day). This gave my children a two for one deal and I would have more time to recover from chemo and enjoy the moment a lot more.
It did however not stop my family from having a small celebration and find clever ways to cover up my very large head-covering bald spot.

CT Scan with Contrast, 4 June 2019
In order to see if the chemotherapy did its job, the oncologist had ordered a CT scan with two types of contrast. Firstly, I had to drink two pints of banana-flavored barium sulfate before going to the imaging center and secondly, they gave me more intravenous contrast fluid at the center. As you might imagine, drinking the barium sulfate did no go very well and I had another episode of mental nausea. I never told the medical staff that half the stuff came back out and luckily nobody yelled at me. I guess I had enough nuclear waste in me to take beautiful pictures.
My oncologist was very happy with the scan results. The cancer did not spread to other parts of the body and the bladder area was almost clear of cancer cells. Given that the bladder will be removed anyway, all of this was good news and he believed the treatment had achieved the intended goals.
The oncologist turned me back over to my urologist who will perform the bladder removal and reconstruction surgery. I will have to go back to the oncologist in September to see if the blood clots caused by the first PICC line are still there. If they have "dissolved", I can stop taking the blood thinners. If not, I guess I'll be on my way to a cardiologist.
Father's Day, 16 June 2019
Three weeks after the last chemotherapy it was time to properly celebrate my birthday and Fathers Day. As this was the longest period without chemo treatment so far, I could definitely feel the difference. By getting physically and mentally stronger, I was able to enjoy the day and I even started to properly taste food and drinks again. It was a good day and I even treated myself to a beer. After being sober for a couple of months, I could definitely feel the "cheap date" effect.
Chemo and the Digestive Tract, 19 June 2019
Throughout this blog, I've hinted at the effect chemo has on the digestive tract. Now that my aggressive MVAC chemo is over, let me describe the complete experience. Cancer cells are fast growing and chemo is designed to attack them. Other healthy fast growing cells in your body also become victims during chemo and my digestive tract was affected significantly.
Starting with my mouth. Once I started chemo, the mucous lining of my mouth was impacted immediately and it started to turn over rapidly. For over two months, my mouth felt like it was recovering from a mouth burn and I constantly had that slimy coating everywhere. Luckily I never developed mouth sores which are very common in chemo patients. My tongue saw the biggest effect as my sense of taste changed rapidly. For the first time in my life I started to enjoy (American) sweets as my ability to taste sugar was severely reduced. Bitter and sour flavors were enhanced while salt was harder to taste. As a result, many food items just did not taste right. This was not a constant as it changed during the chemo, driving me mad as the things I liked one week might not be so good the following week. On top of that, I think it was the constant metallic taste in my mouth that affected me the most.
The mucous in my esophagus was also effected but it did not bother me until the end of chemo. On more than one occasion, medication would get stuck and I would have to eat solid foods afterwards to "push" the pills down. In the end this was not such a big deal as I just started to take my medication before meals.
My stomach was clearly affected the most. Before chemo, I occasionally suffered from indigestion and acid reflux but chemo made this a lot worse. Luckily, over the counter antacids and acid reflux medication worked well, so this was also controllable. The biggest issue was the nausea that I already mentioned. Especially towards the end of the chemo treatment, feeling sick to my stomach and vomiting started to happen more often. The prescribed anti nausea medication helped a little but it could not completely bring it under control.
My intestines were the most unpredictable during the process. For no reason I ever discovered, I would go from normal to constipated to diarrhea a few times a week without a noticeable pattern. Although annoying, it was manageable as long as I didn't make any assumptions.
The last thing to mention is that the entire digestive tract became very sensitive to spices. As a person who loves spicy oriental foods, it was interesting to see that within one week of starting chemo, I had to classify black pepper (yes, black pepper) as too spicy for me to handle.
All in all, it wasn't until about six to eight weeks after the final round of chemo that all the symptoms mentioned above went away.